Causes and symptoms of internal hemorrhoids
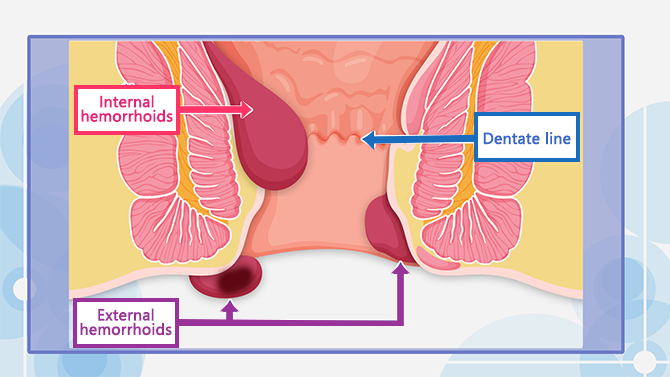
There is an elastic tissue called “anal cushion” that prevents stool and gas from leaking. This anal cushion has rich vascular supply and if it is hurt for some reason, the blood vessels become swollen. This is called “Ibo-Ji” or hemorrhoids. Hemorrhoids that form inside the rectum (inside the dentate line) are called “internal hemorrhoids”, and hemorrhoids that form on the skin around the anus (outside the dentate line) are called “external hemorrhoids”. Generally, when we say “Ibo-Ji” in Japanese, we often refer to internal hemorrhoids.
Internal hemorrhoids are not painful because there are no nerves that feel pain in the rectal mucosa inside the dentate line. However, when the hemorrhoid grows bigger and prolapse outside the anal canal, you may feel dull pain.
Internal hemorrhoids are easily damaged because the rectal mucosa is very soft and delicate. They tend to bleed during bowel movements. Bleeding can be small, but in some cases, it can be large enough to fill the toilet bowl with bright red blood. You may also feel some itchiness or have stains on your underwear from rectal mucus.
Conditions and lifestyles that may lead to hemorrhoids
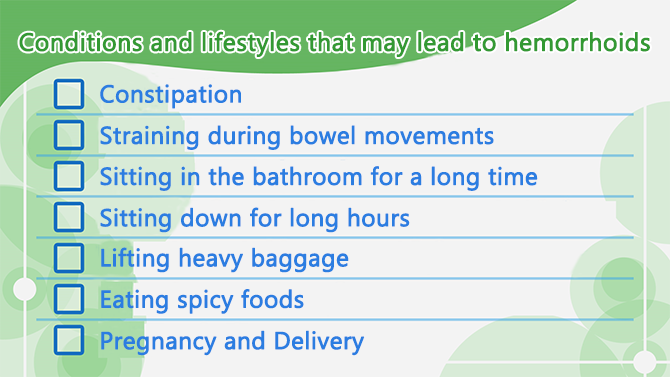
People with the above conditions should be careful because these put excessive straining on the anal cushion and may lead to hemorrhoids.
Treatments and degree of progression
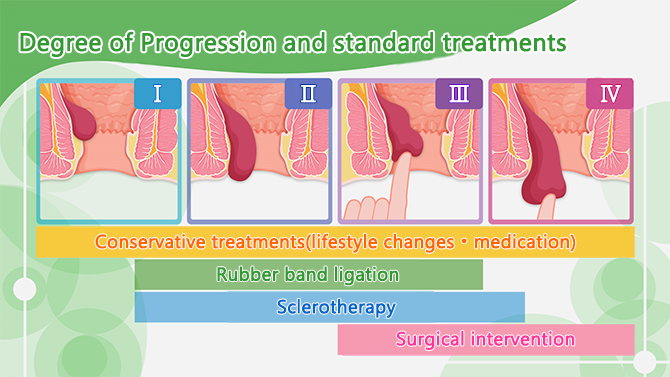
Internal hemorrhoids are classified on a scale of Grade I-IV.
Grade I
Grade I hemorrhoids may bleed but do not prolapse outside the anus. It can be delt with by conservative treatments such as medicines (suppository and ointments) and lifestyle improvements.
Grade II
Grade II hemorrhoids are bigger and may prolapse during bowel movements, but then goes back spontaneously by itself. Treatments include conservative treatment, rubber band ligation and sclerotherapy.
Grade III
Grade III hemorrhoids protrude outside the anus and need to be pushed back in with a finger. Treatments include rubber band ligation, sclerotherapy, and surgery.
Grade IV
Grade IV hemorrhoids are constantly prolapsed and do not reduce when pushed back in with a finger. In many grade IV cases, surgery would be the main treatment option.
Conservative treatments such as medication and lifestyle changes are very important to prevent the progression and recurrences of hemorrhoids. Try to relieve constipation and avoid straining the anal cushion.
Rubber band ligation
Rubber band ligation involves applying a small rubber band at the base of the internal hemorrhoid with a special tool. This restricts blood flow and eventually causes the hemorrhoid to become necrotic. The hemorrhoid will naturally fall off within one week along with the rubber band. This treatment does not require anesthesia nor hospitalization and is relatively painless. However, if the hemorrhoid is either too big or too small, this procedure cannot be done. Also, for patients taking anticoagulant medicine, this procedure cannot be done because of high risk of secondary bleeding.
Sclerotherapy (injection)
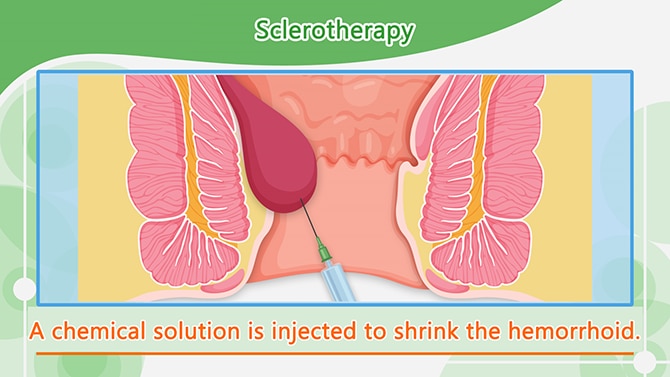
Sclerotherapy is a treatment that involves the injection of a chemical drug into the root of the hemorrhoid which causes it to shrink. This prevents the hemorrhoid from bleeding and prolapsing.
The procedure may be done without hospitalization, but in most cases it requires hospitalization for about 2 to 3 days.
Surgery
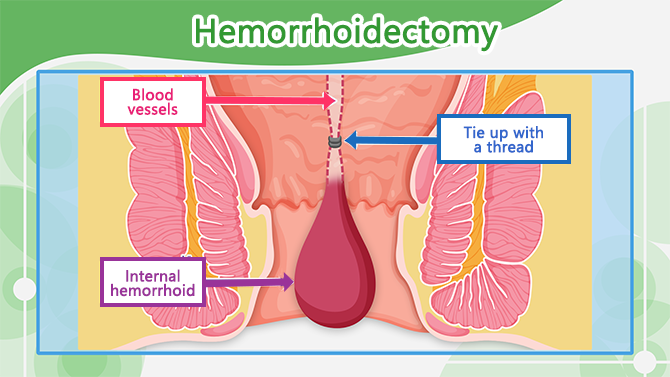
The most common surgery for hemorrhoids is “hemorrhoidectomy”. First, the blood vessel leading to the hemorrhoid is tied to stop the blood flow. Then the excessive tissue is cut off. This procedure usually requires 1 to 2 weeks hospitalization.
Surgery is for grade IV hemorrhoids as well as grade II and III when there is constant bleeding and severe anemia or when it is difficult to reduce the prolapsed hemorrhoid.
You can resume to your normal life such as bathing, a day after surgery. However, avoid heavy exercise, cycling, traveling, sitting for long periods of time, eating spicy foods, and drinking alcohol for 2 weeks after surgery.
Anal fissures: causes and symptoms
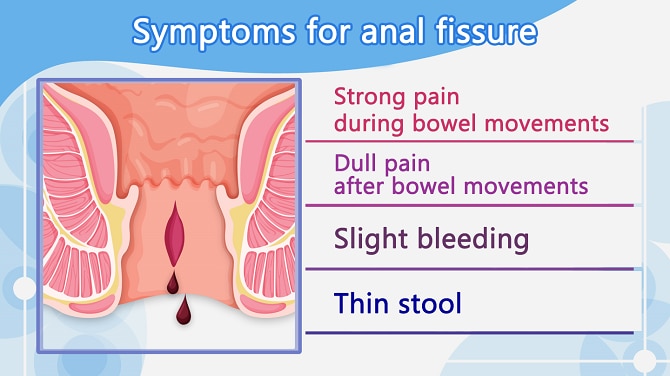
Anal fissures are often confused with hemorrhoids because they have similar symptoms. An anal fissure is a small tear in the lining of the anus. Straining or passing hard stool damages can cause the tear and this leads to bleeding and strong pain during bowel movements. When anal fissures become chronic, the anal canal may shrink and cause dull pain even after bowel movements. Thin stool is also a sign of chronic anal fissure.
The main cause of anal fissure is constipation. Anal fissures are more common in women because women are more likely to have constipation than men. Younger people (20’s-50’s) are more likely to have anal fissures.
Home remedies for anal fissures
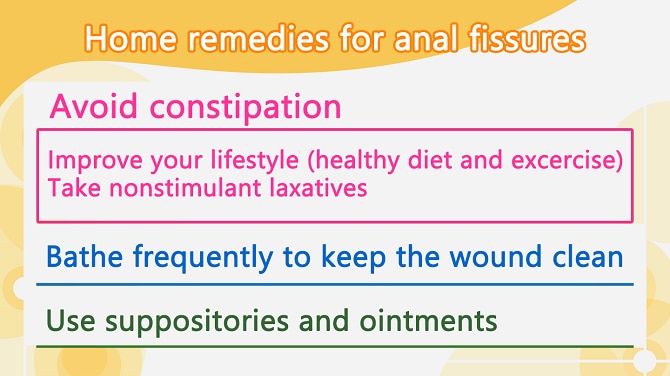
Anal fissures can often be improved with self-care. The most important thing is to relieve constipation. Try to improve your lifestyle such as eating and exercising to improve your bowel movements. When taking non-prescribed laxatives, use nonstimulant laxatives to soften the stool.
Keep the wound clean by taking a bath. If you have pain, use over-the-counter suppositories or ointments to relieve your symptoms.
Surgical interventions for anal fissures
You may consider surgery if you have recurrent fissures. You may also want to consider surgery if you are reluctant to go to the bathroom because of strong pain during bowel movements.
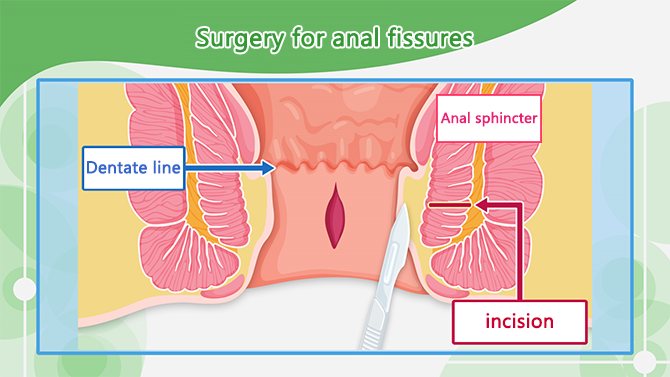
Surgery includes making a small incision (less than 1cm) in the anal sphincter to widen the anal canal.
